IVF to Baby, and Everything In Between
A Mother and Genetic Counseling Student’s Personal Testimony
Written by: Orin Whitby
My fertility journey began when my husband and I started trying to conceive in early 2018:
I had always suspected I would have issues conceiving because of the extreme irregularity of my menstrual periods, so after attempting to conceive naturally for about 8 months, I asked my gynecologist for testing. My doctor was hesitant. They said it had still been under one year, which is within the normal range of time it can take for couples actively attempting pregnancy to conceive, but agreed to prescribe me Clomid, which is an ovulation-stimulation medication; a daily pill that is meant to increase ovulation.
I took it for six cycles, each cycle lasting about two months, and throughout the year of medication, my body failed to ovulate. My doctor decided to refer me to another clinic for a hysterosalpingography (HSG) test, in which a dye is injected into the uterus through a catheter that can be seen flowing into the fallopian tubes on an ultrasound. If it does not flow into the tubes, that indicates that the tubes are blocked, meaning a natural pregnancy could not be achieved. However, the dye flowed through both tubes, revealing mine were open.
After more blood work and a referral for my husband for sperm analysis, I raised a concern about polycystic ovarian syndrome (PCOS). I had heard and read a lot about it and thought it might match my situation. My doctor believed I did not fit the typical presentation of PCOS, so he had never tested me for it, but after advocating for my concerns, he agreed to run the test. Once I was finally checked, the diagnosis for PCOS was immediate.
Polycystic Ovarian Syndrome (PCOS) and Conception:
An ultrasound of my ovaries showed many of cysts on both, blood work showed very high levels of Anti-Mullerian hormone (AMH), and my irregular periods also aligned with the condition. When the doctor confirmed that I have quite a severe form of PCOS and that I would absolutely need IVF to become pregnant. I was happy to finally have a diagnosis, yet sad to realize that I would need a lot more blood tests, ultrasounds, and many hormone injections to conceive. Plus, the financial costs of IVF terrified me.
I found a reproductive endocrinologist (RE) who specialized in fertility and we met for an initial consultation. My husband and I went over our medical history and explained our goals and expectations. He referred me for some more diagnostic testing to complete my profile, and then we were good to go!
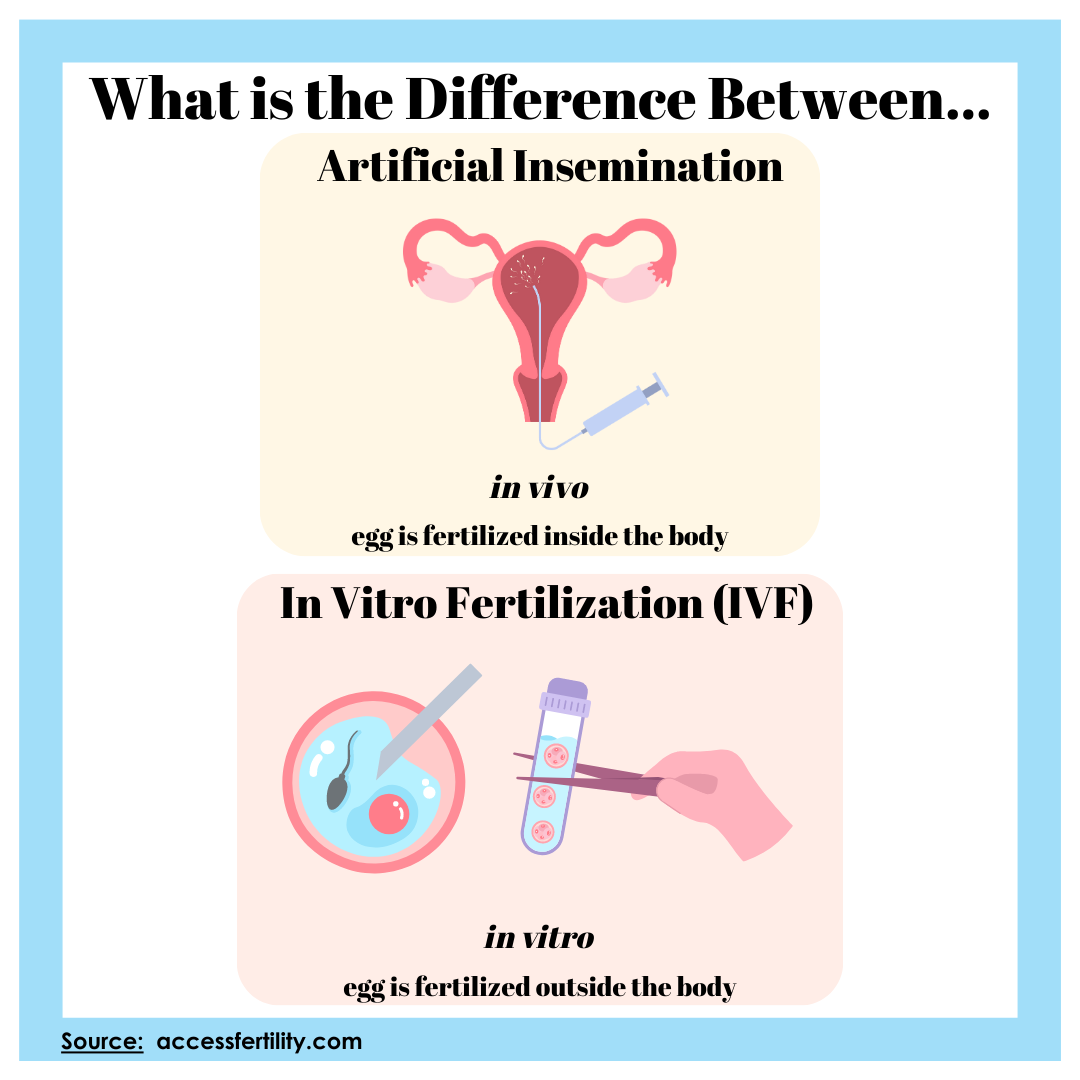
We started with an artificial insemination cycle, which I came to with very low expectations.
The only medication used during the insemination were letrozole pills to induce ovulation. I ovulated, for likely, the first time in my life! Yet, the cycle failed. So I told my fertility doctor that I was ready to proceed to in-vitro fertilization (IVF); I did not want to waste any more time or money on procedures with low success rates. So we did.
Beginning IVF:
In February 2020, we started our first IVF cycle.
After paying about $26,000 in advance to begin the cycle, for about two and a half weeks I received:
3-4 daily hormone injections into the lower abdominal area,
twice weekly blood tests,
and ultrasounds every 2-3 days to follow follicular development
Finally, we were ready for egg retrieval. About 36 hours before the retrieval, I had to inject an hCG trigger shot to help the follicles mature. I was sedated during the very short egg-retrieval procedure.When I awoke the doctor told me how many eggs they extracted. While I was in the surgery room, my husband was called to another room for sperm collection. Then, the eggs and sperm were taken to the embryology laboratory and were immediately fertilized.
By the end of the day we received an update from the lab about the amount of successful fertilizations. Because of my PCOS, I produced way too many follicles, 70, out of which only 49 eggs were retrieved. 47 were mature oocytes, 36 were fertilized, and finally on the fifth day, we ended with 6 blastocyst embryos.
All 6 were biopsied for the preimplantation genetic testing for aneuploidy (PGT-A) and immediately frozen in a process called cryopreservation.
The results came back a week later: one euploid 46 chromosome male embryo, one low mosaic male embryo, one aneuploid embryo, and three embryos yielded no results. We were asked to sign a consent for a re-biopsy of the three no-result embryos, which we did, but they all died in the thaw before the re-biopsy. We agreed to donate the chromosomally atypical embryo for research, and kept the typical and mosaic embryos.
COVID-19 just hit the United States and my clinic shut down for three months. In the meantime, my husband and I talked and decided that we want more than 2 kids, so we should do another IVF cycle before a transfer to take advantage of my younger eggs. In May 2020, we underwent the second round of IVF and had similar numbers: 65 follicles, 38 mature oocytes, 29 successfully fertilized, and only 3 survived to the 5th day. We again chose to PGT-A test them, and a week later learned that one was an aneuploid male and the other two were 46 chromosome females.
Orin’s PGT-A results from her first IVF cycle in February 2020.
Orin’s PGT-A results from her second IVF cycle in May 2020.
Complications of PCOS and IVF: Ovarian Hyperstimulation Syndrome (OHSS)
Unfortunately, because of my PCOS I am prone to Ovarian Hyperstimulation Syndrome (OHSS), which happened after both egg retrievals. OHSS is the most painful thing I have ever experienced. My belly swelled up and I looked 6 months pregnant, which felt like A LOT of painful pressure inside my body. I could not move without feeling the pain. Accompanying the swelling was five-days of ongoing constipation, dehydration, nausea, and vomiting. It was all over after the tenth day post-retrieval.
Transferring the Embryos:
By this point, we had four embryos in cryopreservation. The following month, we started a frozen embryo transfer (FET) cycle. We selected the healthiest male from the first transfer. The cycle took approximately three weeks, I had a few vaginal ultrasounds to monitor the increasing thickness of my uterine lining along with blood tests. I was put on oral estradiol pills and intramuscular progesterone in oil (PIO) injections. Together, these two drugs provided the hormonal support, which I was to continue taking until the tenth week of pregnancy following implantation.
On transfer day I came in with a full bladder, as requested, because it helps the ultrasound gain a better view of the uterus. The procedure required no anesthesia and only took a few pain-free minutes. The embryo was injected into the uterus through a catheter, and I was thrilled to witness this visibly on the ultrasound monitor.
Ten days later, I came back for a beta-HCG blood test. A few hours later, my doctor called to congratulate me. I was pregnant.
I continued having ultrasounds and blood tests until I was officially 10 weeks pregnant, and then I “graduated” from the fertility clinic and switched over to see a regular Obstetrician. Regardless of what was considered a healthy pregnancy, the long and painful experience with trying to become pregnant caused me to experience prenatal anxiety almost constantly throughout the pregnancy.
Labor, Delivery, and Post-Partum Reflections:
At 39 weeks and 4 days, I went into labor. 28 hours later, my son was born. Labor and delivery were both fun and easy experiences for me, contrary to what I had expected. After more than two years of trying to conceive and nine months of anxiety, I was so ready to meet my son. The hypnobirthing course I took in the week prior and the epidural made it a pain-free and smooth experience. The prenatal anxiety haunted me until the very last moment, and when I heard his cry for the first time I was so relieved; all of my stress was instantly gone.
My postpartum experience was difficult. Breastfeeding was hard and painful, having to hold my baby day and night for months because he would cry the moment I put him down was exhausting. Sleepless nights triggered anger and symptoms of depression. Nonetheless, I took all the help I was offered, I napped every minute I could, I took walks with the stroller and tried to leave the house as much as possible. Sunshine and fresh air always make my mood better. Focusing on the happy moments has helped me get through the tough times. When I was in the midst of the postpartum struggles, I sought out resources and help for new moms. I joined online support groups and Facebook groups, made more mom-friends at the park or on social media, watched webinars about infant sleep and development, and even talking about it with my partner, friends, and family helped tremendously.
My son is now over 2 years old and the older he gets, the more I enjoy him. He has his own opinions now, he can communicate and understand us, he is playing more independently, and it’s just overall easier than the infancy period. Sure, there are many struggles too, the tantrums are not the best part of my day, but it is so worth it.
About the Author:
Orin was born in central Israel and grew up in Rosh Ha’ayin. In 2014 she met her partner and in 2017 they married and moved to Las Vegas, Nevada. She attended University of Nevada Las Vegas and earned her Bachelor’s of Science in Microbiology in 2021. Orin now lives in Los Angeles, California with her husband, son, and mother-in-law. Orin was accepted to Keck Graduate Institute’s Genetic Counseling Program and will begin her program in fall 2023 working toward her Master’s Degree in Human Genetics and Genetic Counseling, with the goal to become a prenatal and fertility genetic counselor so that she can continue to help other prospective parents complete their journeys.