Patient Accessibility and Neuromuscular Disorders: A Personal Care Attendant’s Perspective
Written By Joan Kornkven, Genomics Correspondent Intern
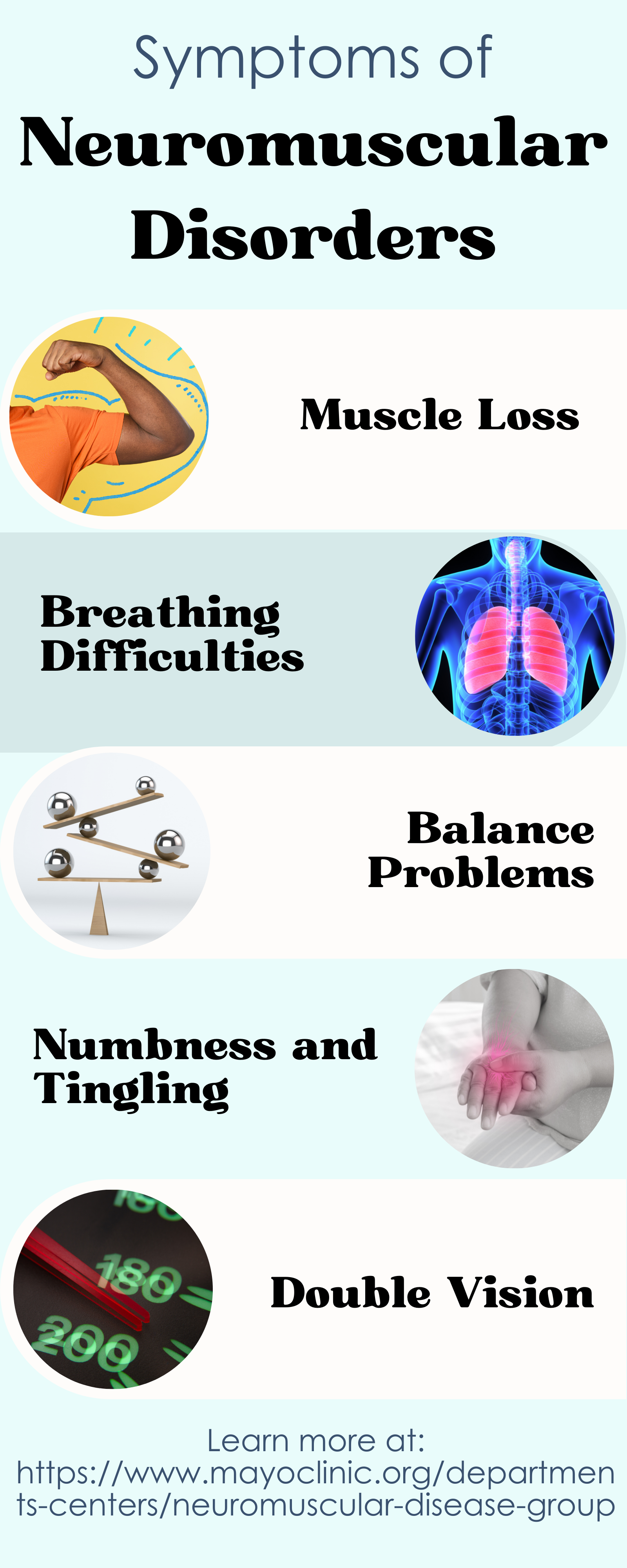
Neuromuscular disorders are a result of improper function between the nerves that control muscle function, which results in problems with the muscles such as weakness, muscle loss, movement issues, trouble with balance, swallowing, and breathing (1). These disorders are caused by changes within certain genes that result in the production of non-functional proteins (1). There are different types of neuromuscular disorders, and they range in severity. Some examples of neuromuscular disorders are: Amyotrophic Lateral Sclerosis (ALS), Multiple Sclerosis (MS), over 30 forms of muscular dystrophy, and Spinal Muscular Atrophy (SMA) (1). Individuals with SMA can have little to no control of their movement and may require a power wheelchair and assistance 24/7.
There are four primary types of SMA that range in severity and age of onset. SMA Type 1 is the most common and severe. It is usually diagnosed within the first 6 months of life, and patients experience muscle weakness and trouble breathing. SMA Type 2 is slightly less severe and is usually diagnosed between 6 months to 2 years of age. Individuals with SMA type 2 cannot walk and require a wheelchair. Individuals with SMA Type 3 are typically diagnosed between 18 months and 3 years of age. While individuals with Type 3 are initially able to walk, motor skills decrease as they get older and many lose this ability. SMA Type 4 is the least severe. It is diagnosed later in life and includes mild motor impairment (2).
I have been working as a personal care attendant (PCA) for a woman with SMA since June 2021.. My experience as a professional caregiver opened my eyes to the countless accessibility issues that people with neuromuscular disorders face on a daily basis. The responsibility of advocating for the importance of accessible healthcare is on those working within the medical field. As a future genetic counselor, I believe it is vital that healthcare providers are aware of the challenges their patients face when navigating barriers to attend appointments in order to ensure they have a full understanding of their patient’s experience.
Easy access to healthcare appointments is a major issue for people with neuromuscular disorders. They require a team of specialists who are thoroughly educated on their condition to provide the best personalized care and treatments specific to their needs (3). As a PCA, I attended numerous appointments to see a range of specialists including occupational therapists for wheelchair fittings, physical therapists, pain specialists, pulmonologists, and specialized neurologists that are highly trained in managing SMA. With so many required appointments, patients with neuromuscular conditions are going to medical clinics and appointments significantly more often than most. However, the need for specialists to deliver care means that there are not many hospitals that can provide the care these people need. This means that many patients are left to face substantial accessibility issues. Patients may live far from a specialty clinic, lack transportation, or may be unable to take time off work (3). An issue I have seen first-hand is a lack of PCAs available to take my employer to her appointments. This meant that she had to work around her own availability, the clinic’s availability, and the availability of her PCAs.
Unfortunately, difficulty finding caregivers is a common and critical issue that people with neuromuscular disorders face. Without a caregiver, someone with a condition like SMA would not be able to prepare their own food, use the restroom, get into bed, or leave the house. The woman I care for consistently struggles with finding full PCA coverage. She requires help 24/7 and would ideally staff five full-time PCAs. However, because the majority of her PCAs are very part-time college students she uses a team of about ten caregivers to cover all of the care shifts. During the time I worked for her she was almost always short staffed. This meant her 70-year-old father would have to step in and care for her when no PCAs were available.
Not having consistent caregivers is a huge barrier for people with neuromuscular disorders, yet it is very common. During an informational interview on the realities of organizing care for individuals with neuromuscular disorders, medical social worker Mark Schmertmann, MSW, LSW, explained:
“the lack of caregivers available may largely be attributed to a lack of funding from states to pay caregivers. Taking care of someone with a severe neuromuscular disorder is hard and stressful work. It requires hands-on, physical, and intimate care. Thus, quality care is dependent on how hard someone is willing to work for low pay. Many people look to hire college students who want experience in healthcare.”
However, the high level of responsibility, attention to detail, compassion, and physical demands of the job warrants an income far higher than the average PCA wage of $14.07 an hour (4). More funding is needed to pay caregivers a desirable wage to fix the issue of a lack of caregivers.
Transportation is another pressing accessibility issue that is critical for participation in society. People that use a powerchair require special vehicles to travel, which can be expensive. Although there are many laws and programs in place to make transportation accessible, there are still gaps that need to be solved (1). Older adults with mobility issues tend to choose personal vehicles over public transportation due to inaccessible vehicles, restricted services, and lack of availability, especially in rural areas (1). Not only do people with disabilities have difficulties accessing vehicles and public transportation, but traveling short distances in their chair can be challenging. Traveling over a bumpy sidewalk in a wheelchair is often uncomfortable and potentially dangerous for someone with a neuromuscular disease who is unable to control and tense their muscles when hitting a bump. It is important for people with disabilities to have access to basic transportation needs. As it stands, current options are not enough.
The increased use of telehealth visits may act as a patch for some of these issues. It allows people to communicate with their doctors and care team more frequently without the barriers caused by travel and is usually less expensive (5). However, it also raises other problems. Some patients may not have access to high-speed internet, or a device to make a call. Further, some patients have concerns about the privacy of health data through technology, which can vary depending on what platform is used for the call (5). Lastly, many appointments people with neuromuscular conditions attend require a physical exam or hands-on approach, thus telehealth visits are not always an option.
Clearly, there are a multitude of accessibility issues that those with neuromuscular disorders face everyday. From inconveniences such as driving over a bumpy sidewalk, difficulty acquiring a fully accessible vehicle, or even being completely unable to attend a required medical appointment due to lack of transportation. It is important for those who are familiar with this subject to advocate for improved and broader accessibility, as many people are unaware that these problems still exist. As a society, we must continue to work on accessibility in all areas of life to ensure the best quality of life for people with disabilities.
Works Cited
Remillard, E. T., Campbell, M. L., Koon, L. M., & Rogers, W. A. (2022). Transportation challenges for persons aging with mobility disability: Qualitative insights and policy implications. Disability and Health Journal, 15(1, Supplement), 101209. https://doi.org/10.1016/j.dhjo.2021.101209
Admin. (n.d.). Types of SMA. Cure SMA. Retrieved May 31, 2022, from https://www.curesma.org/types-of-sma/
Friday, K. D. B. |, May 14, & 2021. (2021, May 14). Breaking Healthcare Barriers. Muscular Dystrophy Association. https://www.mda.org/quest/article/breaking-healthcare-barriers
Home Health and Personal Care Aides. (n.d.). Retrieved June 2, 2022, from https://www.bls.gov/oes/current/oes311120.htm
Watson, S. (2020, October 12). Telehealth: The advantages and disadvantages. Harvard Health.https://www.health.harvard.edu/staying-healthy/telehealth-the-advantages-and-disadvantages
Print. (n.d.). Neuromuscular Disease—Overview. Mayo Clinic. Retrieved May 9, 2022, from https://www.mayoclinic.org/departments-centers/neuromuscular-disease-group/overview/ovc-20443670